What is Delirium Tremens (DTs)?
Delirium tremens, commonly known as DTs, is a severe and potentially life-threatening form of alcohol withdrawal. It requires immediate medical attention and can occur when someone with a physical dependence on alcohol stops drinking.
Quick Answer:
- Definition: A serious medical emergency resulting from abrupt alcohol cessation in dependent individuals.
- When it occurs: Typically 48 to 96 hours after the last drink, but can be up to 10 days later.
- Key symptoms: Severe confusion, hallucinations, tremors, rapid heart rate, high blood pressure, fever, and seizures.
- Who is at risk: Those with a history of heavy, prolonged alcohol consumption and previous withdrawal episodes.
- Prevalence: Affects 3 to 5% of people in alcohol withdrawal; can be fatal without treatment.
- Treatment: Requires hospitalisation for medication, monitoring, and supportive care.
DTs is the most severe stage of alcohol withdrawal. After prolonged heavy drinking, the brain adapts to alcohol’s presence. When alcohol is removed, the brain becomes dangerously overactive.
This is a critical condition, not just simple discomfort. It can lead to life-threatening complications like seizures, irregular heartbeat, and respiratory failure. Historically, untreated DTs had a mortality rate of 15 to 40%. With modern medical care, this has dropped to 1 to 4%, but only with prompt treatment.
Understanding DTs is vital for anyone with a physical dependence on alcohol. The condition requires professional medical supervision and cannot be managed safely at home.
In Australia, alcohol is the most widely used drug. While many people drink responsibly, a significant number develop alcohol dependence. For these individuals, understanding the risks of withdrawal, including DTs, is crucial for their safety. We provide comprehensive support for alcohol dependence, prioritising well-being.
Understanding Symptoms, Causes, and Treatment
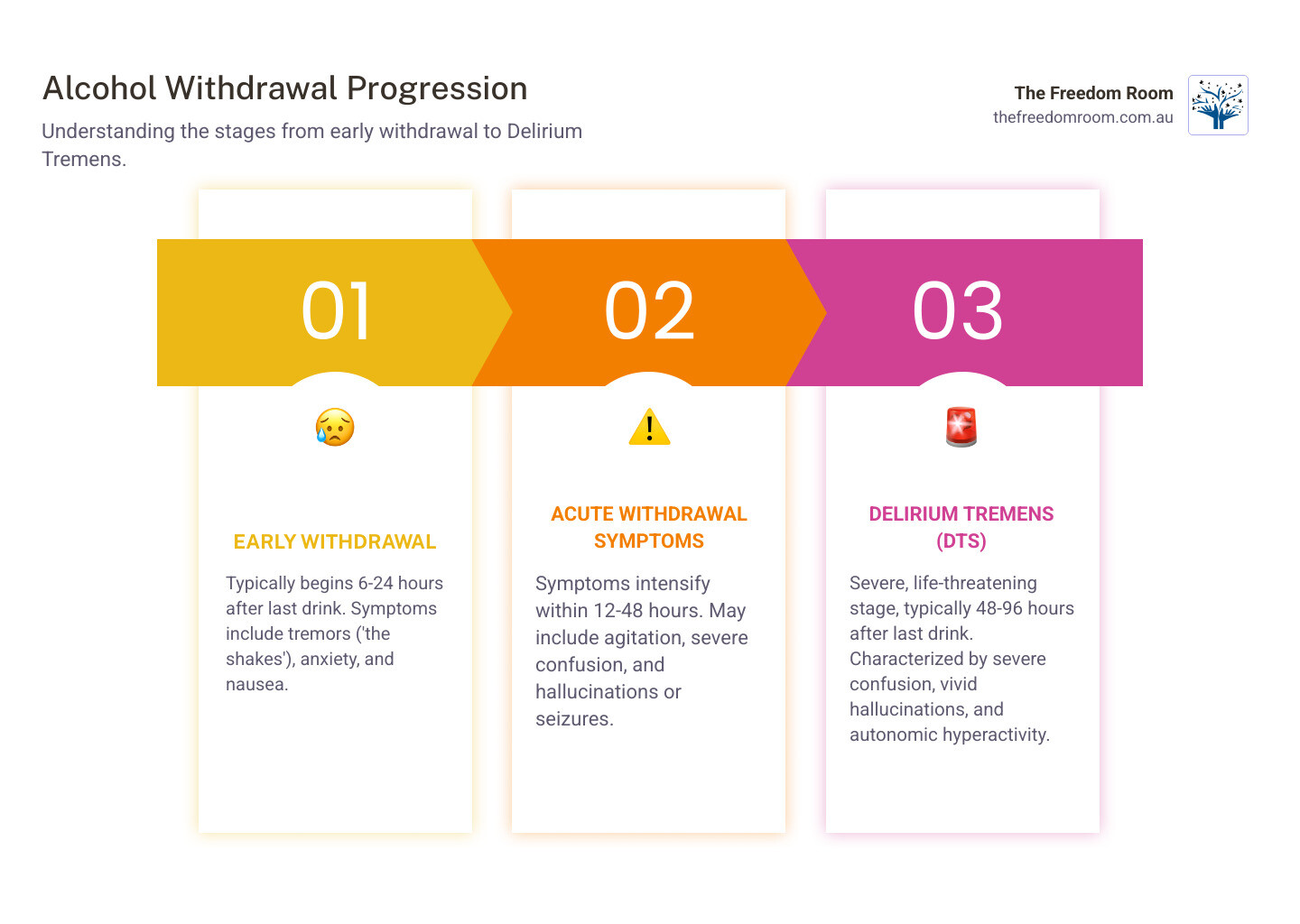
The Progression of Symptoms: From Early Withdrawal to DTs
Alcohol withdrawal symptoms progress from mild to severe. Early signs, appearing 6 to 24 hours after the last drink, include anxiety, insomnia, nausea, and tremors, often called “the shakes.”
Symptoms can worsen over 12 to 48 hours, potentially leading to alcohol hallucinosis (hallucinations without confusion) or withdrawal seizures, also known as “rum fits.” Seizures can occur even without other severe symptoms.
Delirium tremens is the most critical stage, emerging 48 to 96 hours after cessation, but sometimes up to 10 days later. The presence of severe confusion is a key indicator. DTs symptoms are profound and include:
- Severe confusion and disorientation
- Agitation and extreme irritability
- Impaired consciousness
- Vivid and frightening hallucinations (visual, tactile, or auditory)
- Severe autonomic hyperactivity (trembling, sweating, rapid heart rate, high blood pressure)
- Fever
- Nausea and vomiting
- Restlessness
- Sensitivity to light, sound, and touch
These symptoms can fluctuate and become life-threatening without medical intervention.
Causes and Risk Factors for DTs
The cause of DTs lies in how chronic alcohol use affects the central nervous system. Alcohol is a depressant that slows brain activity. Over time, the brain adapts by increasing its own excitatory signals to maintain balance.

When alcohol is suddenly withdrawn, this adapted state leads to an imbalance. The brain’s excitatory systems become overactive, causing the severe symptoms of alcohol withdrawal and potentially DTs.
Several factors increase the risk of developing DTs:
- History of heavy, prolonged drinking: Consuming large amounts of alcohol daily for months or years.
- Previous withdrawal episodes: A history of withdrawal symptoms, especially seizures or prior DTs, is a strong predictor.
- Co-occurring health conditions: Infections, head injuries, liver disease, or pancreatitis can worsen withdrawal.
- Nutritional deficiencies: Lack of vitamins like thiamine and minerals like magnesium is common and increases risk.
- Older age: Older adults may be more vulnerable due to reduced physiological reserves.
- Other medications: Certain drugs can interact with alcohol withdrawal and affect symptom severity.
Recognising these risk factors underscores the need for medical supervision during alcohol cessation.
How is Delirium Tremens Diagnosed?
Diagnosing DTs is a clinical process that occurs in a hospital due to its emergency nature. Healthcare professionals conduct a thorough assessment including a physical examination, medical history review, and diagnostic tests.
A physical exam involves monitoring vital signs for autonomic hyperactivity, such as a rapid heart rate, high blood pressure, fever, and heavy sweating. Staff also observe for tremors, agitation, and mental status changes like confusion.
A detailed patient history is vital, covering alcohol use patterns, time since the last drink, and previous withdrawal episodes. Family or friends may need to provide this information if the patient is confused.
Diagnostic tests help rule out other conditions and assess overall health:
- Blood tests: To check electrolyte levels, liver and kidney function, and blood glucose.
- Toxicology screen: To identify other substances that could complicate withdrawal.
- Electrocardiogram (ECG): To monitor heart rhythm for potential arrhythmias.
- Electroencephalogram (EEG): To evaluate brain activity if seizures are suspected.
The Clinical Institute Withdrawal Assessment for Alcohol, Revised (CIWA-Ar) scale is often used to score symptom severity and guide treatment, though it is not a diagnostic tool for DTs itself.
Medical Treatment and Inpatient Care
Treating DTs is a medical emergency requiring hospitalisation, sometimes in an intensive care unit (ICU) for continuous monitoring. The goals are to save the person’s life, relieve symptoms, and prevent complications.
Benzodiazepines are the primary treatment. Medications like diazepam and lorazepam are used to manage agitation, prevent seizures, and stabilise vital signs by calming the overactive nervous system. Doses are often adjusted based on symptom severity.
Supportive care is also crucial. This includes:
- A calm environment: A quiet, well-lit room helps reduce confusion and sensory overload.
- Reassurance: Verbal reassurance can ease anxiety during periods of confusion.
- Intravenous (IV) fluids: IV fluids are given to correct dehydration and electrolyte imbalances.
- Nutritional support: Thiamine (Vitamin B1) is given intravenously to prevent serious neurological conditions like Wernicke-Korsakoff syndrome. Other vitamins and minerals, such as magnesium and folate, are also supplemented.
If symptoms do not respond to benzodiazepines, other medications like phenobarbital may be used. In severe cases, general anaesthetics might be needed, which requires mechanical ventilation. Any concurrent illnesses must also be treated. Our approach is holistic, ensuring all aspects of the patient’s health are addressed. You can find more scientific research on DTs assessment and management through resources like the National Center for Biotechnology Information.
Recovery Timeline and Potential Complications
The acute symptoms of DTs usually subside within three to seven days of starting treatment. However, some symptoms may persist for weeks or months in severe cases.
After the acute phase, some individuals experience post-acute withdrawal symptoms for a year or more, including:
- Emotional mood swings
- Fatigue
- Sleep disturbances
If not managed properly, DTs can cause serious complications:
- Respiratory failure: Breathing can be compromised by severe agitation or aspiration.
- Cardiac arrhythmias: Life-threatening irregular heartbeats.
- Injury: From falls or self-harm during confusion or seizures.
- Wernicke-Korsakoff syndrome: A neurological disorder from thiamine deficiency that can cause permanent brain damage.
DTs is a serious condition. While historical mortality rates were 15-40%, modern treatment has reduced this to 1-4%. This underscores the importance of immediate medical care.
Preventing Delirium Tremens
The most effective way to prevent DTs is to undergo a medically supervised withdrawal. Stopping alcohol abruptly can be dangerous for those with a physical dependence, so professional oversight is crucial.
A medically supervised withdrawal allows healthcare professionals to manage symptoms with medication, preventing complications like seizures and DTs. This is the safest detox method for anyone with risk factors for severe withdrawal.
Long-term prevention involves a commitment to recovery from alcohol use disorder. Key strategies include:
- Seeking professional support: Engage with services like The Freedom Room for personalised treatment that addresses the root causes of dependence.
- Building a support network: Connect with family, friends, and peer groups like Alcoholics Anonymous (AA) or SMART Recovery.
- Ongoing care: Continuous therapy, counselling, and relapse prevention strategies help develop coping skills and maintain sobriety.
For many, lifelong abstinence is the safest path. Proactive steps and professional support can significantly reduce the risk of DTs and help build a healthier future.
Take the First Step Toward a Fulfilling, Alcohol-Free Life
Recovery from alcohol dependence and preventing complications like delirium tremens is possible. We understand the challenges and offer a path forward rooted in compassion and lived experience. Our team at The Freedom Room in Strathpine, QLD, provides personalised care that respects your unique journey. We encourage you to explore how our alcohol addiction treatment can empower you to achieve lasting sobriety and well-being.
Frequently Asked Questions
Q1. What is delirium tremens (DTs)?
A. Delirium tremens (DTs) is the most severe form of alcohol withdrawal. It is a medical emergency that affects individuals with physical dependence on alcohol who suddenly stop or reduce their drinking.
Q2. What are the symptoms of delirium tremens?
A. Symptoms include severe confusion and disorientation, agitation, aggression, irritability, impaired consciousness, vivid visual, tactile, or auditory hallucinations, heavy sweating, rapid heart rate, high blood pressure, fever, tremors, and seizures.
Q3. What causes delirium tremens?
A. DTs is caused by the brain’s adaptation to chronic heavy alcohol use. When alcohol is suddenly removed, the brain’s excitatory systems become overactive, leading to a state of hyperexcitability in the central nervous system.
Q4. What are the risk factors for developing delirium tremens?
A. Key risk factors include a history of heavy and prolonged alcohol consumption, previous alcohol withdrawal episodes (especially seizures or DTs), co-occurring medical conditions (such as infections or head injuries), older age, and poor nutritional status.
Q5. How is delirium tremens diagnosed?
A. Diagnosis is clinical, based on a physical examination (checking vital signs, observing symptoms), a detailed patient history of alcohol use, and laboratory tests (blood tests for electrolytes, liver function, toxicology screens). Tools like the CIWA-Ar scale help assess symptom severity.
Q6. What are the treatment options for delirium tremens?
A. Treatment requires hospitalisation and often involves:
- Benzodiazepines (e.g., chlordiazepoxide, diazepam, lorazepam) to reduce nervous system overactivity and control symptoms.
- Supportive care, including intravenous fluids for dehydration and electrolyte imbalances.
- Nutritional support, particularly thiamine supplementation to prevent neurological complications.
- Management of any co-occurring medical conditions.
Q7. How long does delirium tremens last?
A. With medical treatment, the main symptoms of DTs usually subside in three to seven days. Some post-acute symptoms, like mood swings and sleep issues, can last for a year or more.
Q8. Can delirium tremens be cured?
A. DTs is not curable, but it is highly treatable. The acute episode can be managed with medical intervention to prevent life-threatening complications. Long-term recovery requires addressing the underlying alcohol use disorder.
Q9. What are the potential complications or side effects of delirium tremens treatment?
A. Complications of DTs itself can include respiratory failure, cardiac arrhythmias, and Wernicke-Korsakoff syndrome. Side effects of treatment are generally related to the medications used, such as oversedation from benzodiazepines, but these are carefully managed in a hospital setting to ensure patient safety.
Q10. How can delirium tremens be prevented?
A. Prevention involves avoiding or significantly reducing alcohol consumption. For individuals with alcohol dependence, the safest way to prevent DTs is to undergo a medically supervised withdrawal. Long-term prevention focuses on treating the underlying alcohol use disorder through therapy, support groups, and ongoing care.


