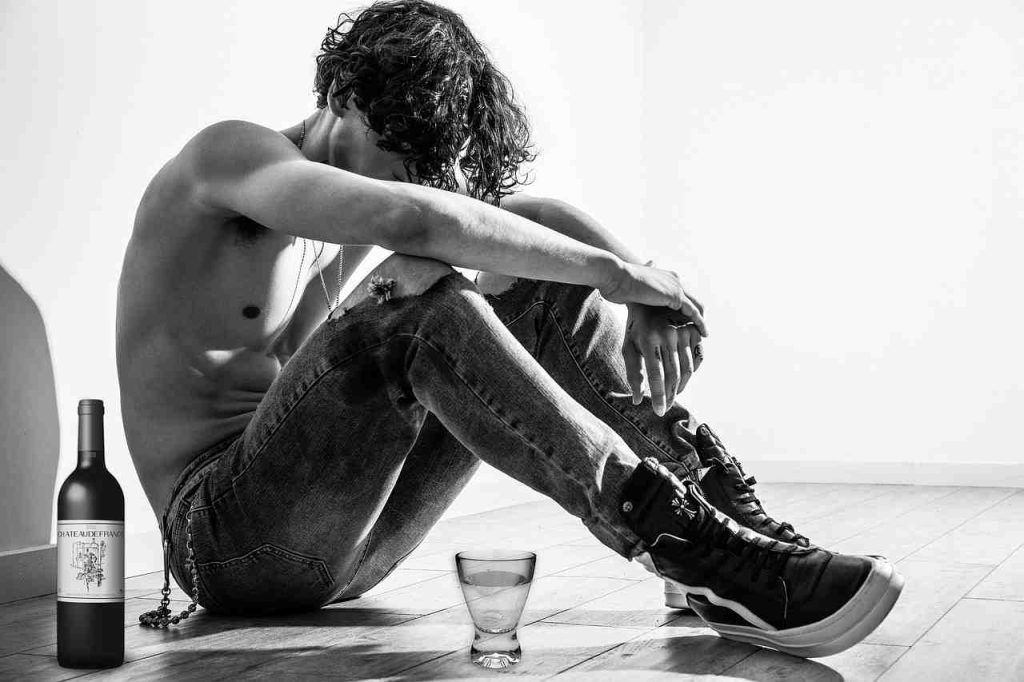
Why Early Recognition of Alcohol Dependence Can Save Your Life
Wondering “What are the early signs of alcohol dependence?” Recognising trouble early is the single most effective way to prevent long-term harm. Alcohol dependence develops gradually, and the first clues are often subtle behavioural shifts rather than dramatic incidents.
Early red flags include:
- Loss of control – drinking more or for longer than planned
- Repeated, failed attempts to cut down
- Rising tolerance – needing extra drinks for the same effect
- Cravings or pre-occupation with drinking
- Neglecting responsibilities at work, home or socially
- Drinking alone or hiding use
- Using alcohol to cope with stress or difficult feelings
- Mild withdrawal signs such as tremor, sweating or anxiety
Dependence sits on a spectrum. Even two or three of these symptoms meet the criteria for mild alcohol use disorder (AUD). Acting swiftly at this point offers the best chance of reversing course without intensive treatment.
In England an estimated 602,000 adults were dependent in 2019, yet fewer than 1 in 10 received help. The earlier you acknowledge concerns, the easier recovery becomes.
If you’re starting to plan evenings around a drink, feel uneasy when alcohol isn’t available, or hear quiet concern from loved ones, now is the time to take stock.
Understanding Alcohol Dependence vs Social Drinking
Social drinking is flexible: you can take it or leave it, go days without thinking about alcohol, and happily decline a round. Dependence means alcohol begins driving your choices. You drink more than intended, feel anxious when you cannot, and start using alcohol to manage stress or low mood.
Dependence is graded:
- Mild AUD – 2–3 symptoms
- Moderate AUD – 4–5 symptoms
- Severe AUD – 6+ symptoms
Using alcohol as a coping tool or bingeing (5 drinks for men, 4 for women, within two hours) are strong indicators you may be sliding along this spectrum.
How Alcohol Hijacks the Brain’s Reward Pathway
Alcohol triggers a dopamine surge in the brain’s reward circuit. With repeated use the brain compensates by producing less of its own dopamine, so you need more alcohol for the same lift – tolerance. Triggers such as finishing work or socialising can then automatically spark cravings.
Genetics account for roughly 60 % of AUD risk. Trauma, chronic stress and mental ill-health further raise vulnerability, explaining why some people progress from social to dependent drinking far more quickly than others.
For evidence-based detail, see Scientific research on alcohol misuse.
What are the Early Signs of Alcohol Dependence?
Changes often appear in your thoughts long before physical withdrawal occurs. You might look forward to the evening drink a little too much or feel unsettled when plans prevent it. Such mental “pull” indicates your brain is learning to rely on alcohol.
Behavioural & Psychological Warning Flags
- Loss of control – intending to have one drink, finishing the bottle
- Secret or pre-loading drinks before gatherings
- Mood swings or irritability when you can’t drink
- Alcohol as the main way to relax or cope
More detail: Warning Signs of Alcohol Dependency
Physical & Tolerance-Based Clues
- Increased tolerance – former “couple of wines” no longer touch the sides
- Morning tremor or slight shakes that settle after drinking
- Sweats, disturbed sleep or night-time waking
- Blackouts or memory gaps on heavier evenings
- Mild withdrawal (anxiety, nausea, poor focus) if several hours pass without alcohol
Seven Practical Ways to Stop Dependence in Its Tracks
Spotting problems early means you can often course-correct with straightforward lifestyle changes rather than formal detox. Combine the strategies below for best results:
- Track your drinking and set weekly limits.
- Schedule alcohol-free days each week to reset tolerance.
- Swap drinking for mood-boosting activities that reduce stress.
- Identify triggers and build coping skills (HALT: Hungry, Angry, Lonely, Tired).
- Speak to a health professional early – brief advice works.
- Use validated self-screening tools to keep yourself honest.
- Build a support network before you hit crisis.
Early intervention is a sign of wisdom, not weakness. Even small changes prove to your brain and body that alcohol is optional – not essential.
1. Track Your Drinking & Set Weekly Limits
Most people underestimate intake. Keep a simple diary or use an app for two weeks, noting drinks, context, and feelings before and after.
UK low-risk guidelines advise no more than 14 units a week, spread across at least three days. (1 pint of regular beer ≈ 2 units; 125 ml wine ≈ 1.5 units; 25 ml spirit = 1 unit.)
If you are well above this, cut back gradually; abrupt change can trigger withdrawal. Consistent tracking builds self-awareness – one of the strongest predictors of long-term control.
2. Schedule Regular Alcohol-Free Days
Give your liver and nervous system time to recover by planning at least two consecutive drink-free days each week. Benefits often appear quickly: deeper sleep, clearer thinking and better mood.
If skipping even one evening feels daunting, that difficulty itself signals early dependence. Use those alcohol-free days to refind enjoyable, relaxing activities that do not revolve around alcohol.
3. Swap Drinking for Mood-Boosting Activities
When alcohol becomes an emotional toolkit, replacing it with healthier options is essential.
- Exercise – even a 20-minute walk releases endorphins that rival alcohol’s short-lived lift.
- Mindfulness or meditation – five minutes of deep breathing can reset stress.
- Creative hobbies – painting, music or puzzles offer focus and satisfaction.
- Alcohol-free social plans – coffee catch-ups, cinema trips or weekend hikes keep connections alive.
4. Identify Triggers and Build Coping Skills
Look for patterns: stressful workdays, social anxiety, or certain places. Use quick tools such as:
- HALT check-in – pause if you are Hungry, Angry, Lonely or Tired.
- Urge surfing – notice a craving, breathe, and watch it peak and pass.
- Grounding techniques – name five things you can see, four you can touch, three you can hear.
Replacing automatic drinking with practical coping strategies weakens the habit loop.
5. Reach Out Early to Health Professionals
Speak to your GP as soon as you suspect problems. Brief interventions – often one or two short sessions – can dramatically reduce risky drinking. Your doctor may:
- Review your diary and agree reduction goals.
- Offer medications such as naltrexone or acamprosate to ease cravings.
- Refer you to counselling or peer-support groups.
Early help is usually simple, discreet and highly effective. More on evidence-based care: Scientific research on early treatment.
6. Use Validated Self-Screening Tools at Home
Quick questionnaires keep you accountable:
- AUDIT (10 questions). Score 8+ suggests hazardous use.
- CAGE – Cut down, Annoyed, Guilty, Eye-opener. Two “yes” answers mean you should seek advice.
- DSM-5 checklist – eleven official AUD symptoms.
They are not diagnoses but excellent prompts for change. For guidance see Do I Have a Problem with Alcohol?.
7. Build a Support Network & Recovery Plan
Recovery is easier with allies.
- Alcoholics Anonymous (AA) – 12-step, peer-led meetings.
- SMART Recovery – evidence-based tools and group support.
- Trusted friends and family – share your plan and ask for practical help.
- Crisis lines – Lifeline 13 11 14 or National Alcohol and Other Drug Hotline 1800 250 015.

Write a simple plan covering goals, triggers, coping strategies and who to call if cravings spike.
Screening Tools, Withdrawal Safety & When to Seek Help
Use your AUDIT score to gauge risk:
- 0–7 : low risk
- 8–15 : hazardous
- 16–19 : harmful
- 20+ : likely dependence – seek professional input
The higher your score and the longer you have been drinking heavily, the greater the risk of dangerous withdrawal. Severe symptoms may include seizures, hallucinations or delirium tremens – all require urgent medical care.
Never attempt to quit suddenly if you have experienced:
- Seizures on previous quit attempts
- Hallucinations when cutting down
- Multiple failed detoxes on your own
In these cases a medically supervised detox is lifesaving. More information: Alcohol Use Disorder.
How to Support a Loved One Showing Early Signs
- Choose a calm, sober moment to talk.
- Use “I” statements (“I’m worried about how much you’ve been drinking”) rather than blame.
- Offer information on self-tests, helplines and local services.
- Set clear but compassionate boundaries to protect your own wellbeing.
Your role is to provide support and information; the decision to change must be theirs.
Frequently Asked Questions about Early Alcohol Dependence
Can tolerance alone mean I’m dependent?
Tolerance is a warning sign, not proof of dependence. Concern rises when it appears alongside cravings, loss of control or withdrawal symptoms.
How quickly do early signs progress to severe AUD?
Progression varies. Genetics, trauma and mental health can accelerate it, but early intervention often halts the slide.
Is it safe to quit “cold turkey” if I notice early symptoms?
If you have no physical withdrawal signs, gradual reduction or stopping may be safe. If you shake, sweat or feel very anxious without alcohol, seek medical advice before quitting.
Ready for Change? Let’s Build a Stronger, Alcohol-Free Future Together
Recognising the early signs of dependence shows courage and self-awareness. At The Freedom Room Wellness and Recovery in Strathpine, QLD, our team combines professional expertise with personal lived experience to offer compassionate, cost-effective care.
Whether you need a brief check-in, structured therapy, or ongoing peer support, we tailor treatment to your goals and circumstances. You do not have to steer this alone.
Learn more or arrange a confidential chat today: Alcohol Dependence. Progress over perfection – every small step counts toward lasting freedom.