Understanding the Hidden Connection Between Loss and Substance Dependency
The Interrelationship of Grief and Addiction
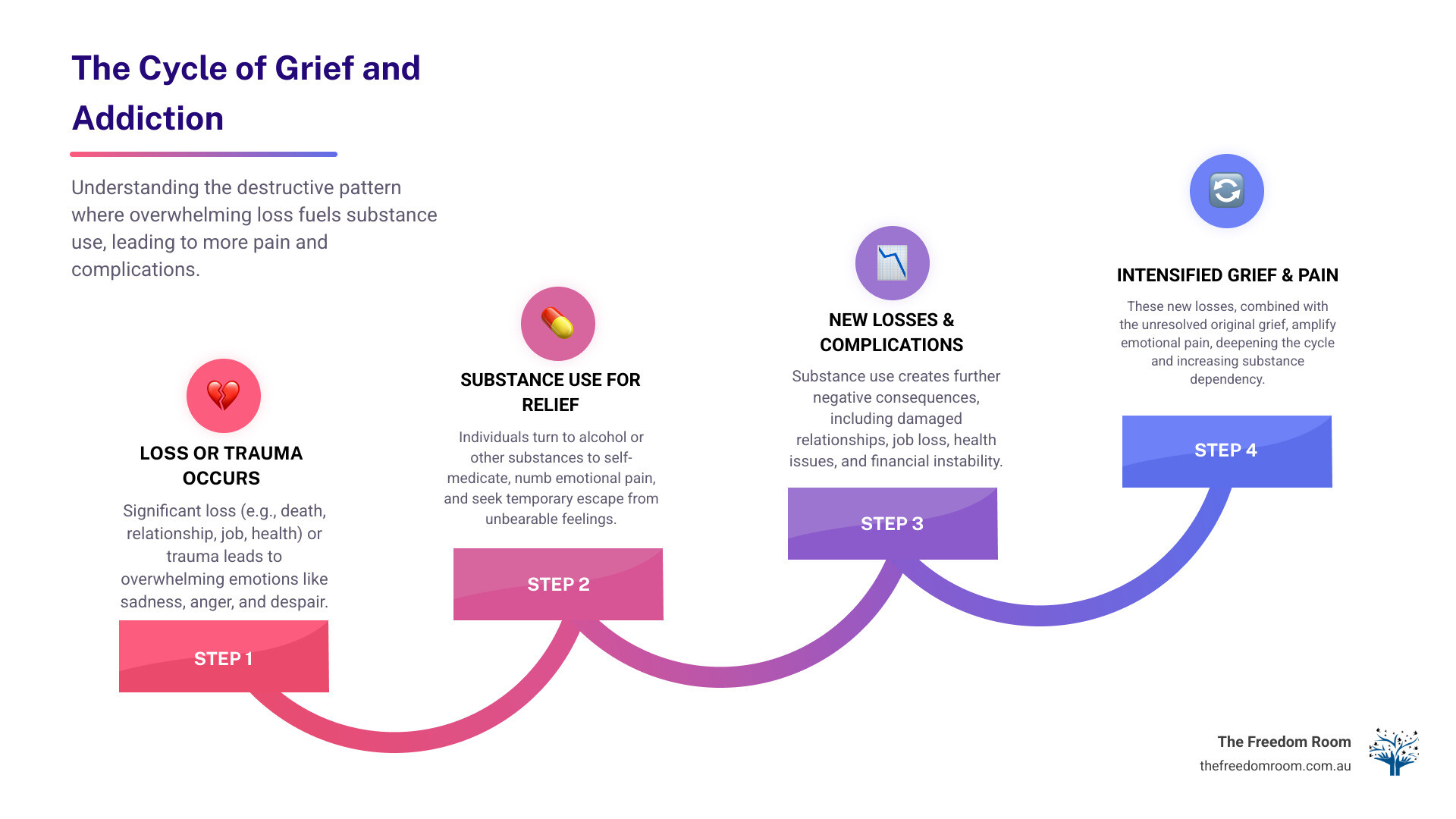
Addiction and grief share a profound and often misunderstood relationship that affects a significant number of Australians. Following a major loss, the resultant emotional pain can lead individuals to use alcohol or other substances for relief. This can establish a detrimental cycle where grief contributes to substance dependency, and the consequences of addiction lead to further loss and grief.
Key Dynamics
Key connections between grief and substance use:
- Self-medication: People use substances to numb overwhelming emotional pain
- Delayed processing: Substances can block the natural grieving process
- Increased risk: Those with existing addictions are more vulnerable to complicated grief
- Higher prevalence: 34.2% of people with substance use disorders show signs of complicated grief, compared to just 5% in the general population
- Bidirectional relationship: Grief can trigger substance use, while substance use can worsen grief symptoms
The Cycle of Self-Medication and Unresolved Grief
Research indicates that grief is a response to any significant loss, not limited to bereavement. It can include the end of a relationship, job loss, declining health, or a diminished sense of identity. The associated emotions of sadness, anger, guilt, and despair can be overwhelming, prompting some individuals to use alcohol or drugs as a coping mechanism.
This pattern of self-medication creates a destructive cycle. While substances may temporarily mask emotional pain, they impede healthy emotional processing. Over time, this can lead to the development of an addiction, leaving the initial grief unresolved and potentially exacerbating both conditions.
The Importance of Integrated Treatment
Recognising this connection is crucial for effective recovery. Unaddressed grief can undermine sobriety and increase the risk of relapse. Therefore, successful treatment must adopt an integrated approach that addresses both the addiction and the underlying grief to facilitate lasting healing.
Understanding the Depths of Grief
The Broad Spectrum of Grief
Grief is a profound and universal human experience, though its manifestation is unique to each individual. While commonly associated with the death of a loved one, grief encompasses a much broader spectrum of significant losses. The dissolution of a meaningful relationship, redundancy from a valued job, a decline in health, or the loss of one’s sense of identity can all precipitate a grieving process.
Emotional and Physical Manifestations
The emotional landscape of grief is extensive and unpredictable, often involving cycles of intense sadness, anger, guilt, or numbness. These feelings do not adhere to a linear timeline, and there is no prescribed manner in which to experience them. It is also common for physical symptoms to accompany this emotional pain.
The body’s response to grief mirrors its reaction to major stress. This can result in persistent fatigue that interferes with daily tasks, and sleep patterns can become significantly disrupted, presenting as either insomnia or hypersomnia. Appetite changes are common, as are headaches, digestive problems, and a general feeling of physical heaviness. Understanding these varied responses is an important step in managing the experience. More info about Emotional Health.
The Five Stages of Grief
Psychiatrist Elisabeth Kübler-Ross introduced a model of grief as a five-stage process in her 1969 work. While this framework is useful for understanding common responses to loss, it is important to note that grief is not a linear process. Individuals may experience these stages in any order, revisit them, or not experience some stages at all. This variability is a normal part of grieving.
The five stages include:
- Denial – The initial shock and disbelief that helps buffer overwhelming pain
- Anger – Powerful emotions that might be directed at anyone or anything, often masking deeper hurt
- Bargaining – The “what if” thoughts and desperate attempts to negotiate with fate
- Depression – Profound sadness and withdrawal as the full weight of loss settles in
- Acceptance – Coming to terms with reality and finding ways to move forward
Denial serves as a protective psychological mechanism, creating temporary emotional distance when reality is too overwhelming to process. This initial shock and disbelief allows for the gradual absorption of the loss.
Anger can be a powerful emotion, sometimes directed at the deceased, oneself, or others. This anger often masks deeper feelings of hurt and reflects the depth of the attachment and the perceived injustice of the loss.
During the bargaining stage, an individual may engage in “if only” or “what if” thinking, reflecting a desire to regain control in a situation that feels chaotic and unmanageable.
The depression stage is characterised by profound sadness and withdrawal as the full impact of the loss is realised. This is a natural response to bereavement, distinct from clinical depression.
Acceptance does not signify being “over” the loss or an absence of sadness. Rather, it involves integrating the loss into one’s life story and finding ways to move forward while carrying the memory of what was lost.
An individual’s experience with these stages is unique, influenced by factors such as personality, support systems, cultural background, and the nature of the loss. Understanding the five stages of grief from Cruse.
The Psychology and Physiology of Grieving
The experience of grief involves complex changes in the brain and body, underscoring its profound impact on an individual’s overall functioning. Understanding these processes can clarify why grief feels so pervasive.
Neurological Activity
Brain activity during grief shows distinct patterns. The amygdala, the brain’s threat detection centre, becomes highly activated, contributing to the intense feelings of sadness, fear, and emotional pain. Concurrently, the medial prefrontal cortex, which is responsible for decision-making and emotional regulation, attempts to process the loss and manage the emotional response. These neurological shifts can explain why executive functions like decision-making may be impaired during grief and why typical coping strategies may be less effective as the brain adapts to a significant life change.
The Stress Response
The body’s stress response system is also highly activated during grief. Stress hormones such as cortisol are released into the system, contributing to physical symptoms like disrupted sleep, appetite changes, and fatigue. While this hormonal response is a natural mechanism for managing crisis, its sustained activation can lead to physical and emotional depletion.
Attachment and Evolutionary Perspectives
Attachment theory offers insight into the profound impact of grief. Humans are biologically wired for social connection. When a significant attachment is severed by loss, the attachment system responds with intense distress, explaining the primal and overwhelming nature of grief. From an evolutionary standpoint, grief may serve important functions. The expression of pain can motivate individuals to seek support from their social group, strengthening community bonds. The grieving process also facilitates gradual adaptation to life after loss, thereby building resilience. This understanding of grief’s biological underpinnings is particularly relevant when considering how addiction and grief can intersect, as substance use can interfere with these natural processes and complicate recovery. A scientific look at the grieving brain. More info about Emotional Wellness.
The Intricate Link Between Addiction and Grief

The profound emotional pain of grief can lead individuals to seek methods for numbing or escaping their feelings. This drive to self-medicate is a significant factor in the intricate relationship between addiction and grief. The use of substances may provide temporary relief from overwhelming emotions, but this coping mechanism delays the natural grieving process.
Substance use can block emotional resolution, preventing individuals from fully processing a loss and adapting to its impact. This may trap individuals in a cycle of unresolved grief, hindering genuine healing. This cycle is a contributing factor to increased mortality rates; for example, standardised mortality rates among opioid-dependent individuals in Australia are significantly higher than those of the general population. Why is Mental Health Important?
How Grief Can Fuel a Substance Use Disorder
Grief, particularly when it is intense or associated with trauma, can be a powerful trigger for the development of a substance use disorder. When faced with the pain of loss, some individuals turn to drugs or alcohol as a coping mechanism to numb their emotional distress. This self-medication offers an immediate, though temporary, escape from overwhelming feelings.
This is especially prevalent in cases of traumatic loss, where unresolved pain may be temporarily soothed by substance use, which in turn can lead to further losses and an escalation of substance use. Research indicates that the likelihood of developing a substance use disorder (SUD) is substantially increased among young adults who experience multiple bereavements in a short period. For many, unresolved grief is a primary factor in the development of addiction, highlighting the importance of grief work in the recovery process. The role of grief in addiction from Psychology Today.
Understanding Complicated Grief and its Connection to Addiction and Grief
Not all grief follows a typical path. For some, the mourning process becomes much longer and more intense. This is known as Complicated Grief (CG). It’s now formally recognised as Persistent Complex Bereavement Disorder (PCBD) in the DSM-5, which is the standard guide mental health professionals use to diagnose mental health conditions. This condition involves persistent and debilitating grief symptoms that make it really hard for someone to adapt to their loss. People with PCBD often stay in the acute, intense phase of grief for an extended period, usually more than six months to a year.
Research clearly shows a significant overlap between CG and substance use disorders. A 2017 study found that 34.2% of individuals with substance use disorders exhibited symptoms of complicated grief, a stark contrast to only 5% in a control group. This indicates that people struggling with SUD are considerably more vulnerable to experiencing complicated grieving. The presence of CG can lead to poor coping mechanisms, often driving individuals deeper into substance use as they attempt to manage their unresolved pain.
Exposure to trauma, whether in childhood or later in life, significantly increases the risk of developing complicated grief disorder. This connection highlights how early life experiences can make individuals more susceptible to both prolonged grief and substance misuse. When individuals lack healthy coping skills, intense grief, especially complicated grief, can lead to increased substance use or relapse as a means of temporary emotional regulation.
More info about Mental Health Relapse Prevention Guide.
The Impact of Grief on Existing Addiction
For individuals with a pre-existing addiction, the experience of grief can be a significant destabilising factor. The emotional weight of loss can exacerbate feelings of hopelessness and despair, potentially intensifying addictive behaviours. This can undermine recovery efforts, increase the risk of relapse, and make it more difficult to maintain sobriety.
Research indicates that the experience of grief and the associated loss of social support can profoundly destabilise individuals with Opioid Use Disorder (OUD), leading to severe outcomes such as overdose and suicide. While substance use may offer temporary relief, it ultimately worsens negative moods in the long term, creating a detrimental cycle.
Gender can also be a factor in how grief impacts substance use. Studies have shown that bereaved men exhibit higher rates of alcohol dependence symptoms and harmful alcohol use compared to non-bereaved men, with this disparity increasing in the second year following a loss. Men were twice as likely to have an alcohol use disorder two years after a loss than men who were not grieving. These findings underscore the importance of gender-sensitive support.
Healthy Coping and Professional Support

When addiction and grief co-occur, the path to healing requires a structured and compassionate approach. Recovery involves learning to process pain with healthy tools and supportive relationships, rather than avoiding it.
Foundational Recovery Principles
Acknowledging and expressing feelings is a foundational component of recovery. Suppressing grief, particularly through substance use, prolongs the healing process by preventing the healthy expression of emotions.
Seeking support networks is essential during this vulnerable period. Connection with trusted friends, family, or support groups can mitigate the isolation that often exacerbates both grief and addiction.
Self-care practices are also critical. This includes prioritising adequate rest, maintaining proper nutrition, and engaging in gentle physical activity to help process the physiological tension associated with grief.
Establishing rituals to honour the loss can also provide a sense of connection and purpose in the grieving process. More info about Emotional Sobriety.
Healthy Coping Mechanisms for Grief
Developing healthy strategies to process grief is protective against the use of substances to numb emotional pain. These strategies do not eliminate hurt but provide constructive channels for the intense emotions associated with loss.
Journaling provides a private, non-judgmental space for articulating thoughts and feelings. This practice can help clarify the complex emotions of grief and allow individuals to track their progress. The Healing Power of Journalling.
Creative expression through art, music, or other artistic forms can give voice to feelings that are difficult to express verbally. These activities facilitate the somatic processing of emotions.
Physical activity, including gentle exercise such as walking, can release endorphins that improve mood and help alleviate the physical tension that accompanies emotional pain.
Mindfulness and meditation practices teach individuals to observe difficult emotions without being overwhelmed by them. These techniques can reduce the intensity of grief and build emotional resilience.
Spending time in nature can offer perspective and a sense of peace. Natural environments can serve as a reminder that healing is a gradual process.
Therapeutic Interventions for Co-occurring Addiction and Grief
Treating grief and addiction as separate issues is often ineffective. An integrated treatment approach that recognises the interplay between these conditions is necessary for lasting recovery.
Individual counselling offers a confidential setting to explore the connections between loss and substance use. A therapist can assist in developing personalised strategies for managing both conditions.
Group therapy connects individuals with peers who share similar challenges, reducing isolation and providing opportunities for shared learning and support.
Support groups, focused on either addiction recovery or grief, offer ongoing community support, accountability, and encouragement beyond formal treatment settings.
Research demonstrates that addressing grief within addiction treatment leads to improved outcomes, including reduced depression, fewer cravings, and greater optimism regarding recovery. A Guide to Addiction Recovery.
How Emotional Freedom Techniques (EFT) Can Help
Emotional Freedom Techniques (EFT), a method involving tapping on acupressure points, offers a structured approach to processing the intense emotions characteristic of both grief and addiction. This evidence-based technique can help regulate the overwhelming feelings that may drive substance use.
The Mechanism of EFT
During distress, our amygdala, the brain’s threat-detection centre, initiates the fight, flight, or freeze response, releasing stress hormones. EFT works by gently tapping on specific acupressure points on the face and upper body while focusing on a distressing thought or emotion. This process sends a calming signal to the amygdala, which helps to down-regulate the body’s stress response and reduce the intensity of the emotional reaction.
The Role of the EFT Practitioner
An EFT Practitioner guides an individual through the process of releasing emotional trauma in a safe and controlled manner. The objective is to process traumatic events so they no longer carry a significant emotional charge, allowing for a new perspective on past experiences without needing to relive them. EFT can be beneficial for the interconnected challenges of addiction and grief, as well as for anxiety, depression, PTSD, and stress management. By disrupting the typical stress-response pathway, regular practice can help retrain the nervous system to respond more calmly to triggers, fostering greater emotional resilience. More info about EFT and CBT Therapy.
Special Considerations: Grieving a Drug-Related Death
The loss of a person to a drug or alcohol-related death results in a particularly painful and complex form of grief. This type of loss often leads to disenfranchised grief, a form of mourning that is not always socially acknowledged, publicly supported, or fully understood. The bereaved may face significant stigma and social exclusion, similar to the experiences of those who have lost someone to suicide.
The resulting isolation can be profound. Unlike other forms of loss where communities often provide support to the grieving family, those experiencing addiction and grief through a drug-related death frequently navigate their pain in isolation due to judgment and misunderstanding from others.
The Hidden Burden Families Carry
For families who were aware of their loved one’s substance use, the period preceding the death is often characterised by prolonged uncertainty, distress, and a sense of powerlessness. This extended period of suffering, sometimes referred to as ‘anticipatory grief’, means that the death can feel like the culmination of numerous smaller losses. The stigma surrounding addiction often compels families to bear this burden in silence, unable to seek support from their usual networks. This isolation compounds the grief, making the eventual loss even more difficult to process.
The Ripple Effect on Children and Young People
Children who lose a parent to a drug-related death face unique challenges. Research indicates these children are at an elevated risk for future substance misuse, particularly when the loss occurs between the ages of six and 18. This can create an intergenerational cycle where addiction and grief can perpetuate. Young people in these circumstances often contend with complex emotions, including guilt, shame, anger, and confusion. They may internalise blame for their parent’s death or feel responsible for the family’s distress. Without appropriate support, these unresolved emotions can contribute to risk-taking behaviours later in life.
The Need for Specialised Support
The grief experienced after a drug-related death requires sensitive and informed care. Traditional grief counselling may not fully address the unique challenges these families face. Support that validates the experience, addresses societal stigma, and helps navigate complex emotions such as blame, guilt, and shame is crucial for healing.
Families require safe, non-judgmental spaces to express the full spectrum of their emotions, which may include relief that a period of uncertainty has ended, alongside profound sadness. It is important that support acknowledges both the love for the deceased and the trauma endured throughout the addiction. The Freedom Room possesses a deep, professional understanding of these complexities, informed by lived experience with addiction, which provides the authentic empathy required to support families through this specific form of grief. More info about Emotional Support for Families.
Conclusion: Pathways to Integrated Recovery
Navigating co-occurring addiction and grief is a complex process that offers the potential for profound healing and sustainable recovery. Understanding the connection between loss and substance dependency is the first step toward breaking the detrimental cycle of pain and self-medication.
Lasting healing requires a comprehensive, integrated approach that addresses both the substance use disorder and the underlying emotional wounds of grief. Recovery is a gradual process focused on consistent progress, not perfection, where challenges are viewed as opportunities for learning and growth.
The Importance of Compassionate, Expert Support
When managing the relationship between addiction and grief, professional guidance is critical. Support from practitioners who understand both the clinical and experiential aspects of these challenges provides a foundation for sustainable recovery.
The most effective treatment models recognise that grief and addiction are not separate issues but interconnected experiences requiring integrated care. This involves working with professionals who can facilitate the processing of unresolved loss while simultaneously developing healthy coping mechanisms for maintaining sobriety.
Recovery Through Lived Experience
At The Freedom Room, our approach is founded on authentic connection and professional understanding. The team combines professional expertise with personal, lived experience of recovery, creating a therapeutic environment conducive to genuine healing.
This combination of evidence-based treatment and experiential insight allows for a unique level of understanding and support. The organisation recognises that each individual’s journey is unique. Treatment is therefore holistic and personalised, addressing the whole person – mind, body, and spirit – rather than just the symptoms of addiction and grief.
Building a Foundation for Lasting Recovery
Recovery from addiction and grief involves developing new methods for emotional regulation, building resilience, and creating meaningful social connections. This foundation supports not only sobriety but also a fulfilling life in which grief can be honoured without becoming overwhelming.
Through personalised sessions and supportive therapeutic modalities, individuals can develop the tools needed for long-term success. The goal is to learn how to navigate difficult emotions without resorting to substances, process loss in a healthy manner, and build a support network that facilitates the recovery journey.
The path forward is not about forgetting loss, but about learning to carry grief in a way that does not undermine one’s life or sobriety. It is about finding meaning, purpose, and well-being alongside healing.
For information on how a compassionate, comprehensive approach can support recovery, explore our holistic addiction recovery programs.

